Differences of tear film osmolarity between two time-points of the day in healthy subjects
Abstract
Purpose: Tear film hyperosmolarity is considered one the core mechanism of the dry eye along with the tear film stability. Many tear physiological variables oscillate during the day. This study was designed to assess the differences in tear film osmolarity between morning and afternoon in a group of healthy subjects.
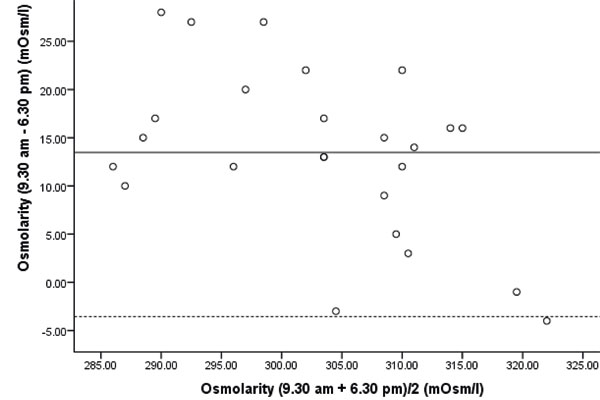
Materials and methods: A total of 25 healthy subjects who fulfilled the study’s inclusion criteria were enrolled for the study. Tear osmolarity was measured using the TearLab™ system in two separated sessions, at 9.30 am and 6.30 pm. A paired t-test and a Bland–Altman test were used to assess the differences between sessions.
Results: Tear osmolarity (mean ± SD) was 309.96 ± 9.00 and 296.48 ± 12.98 mOsm/l at 9.30 am and 6.30 pm, respectively, being significantly lower at 6.30 pm than at 9.30 am (mean difference ± SD = 13.48 ± 8.69 mOsm/l; paired t-test; p < 0.001).
Conclusions: Tear film osmolarity does appear to have some influence by the time of day in healthy patients.
References
Bron AJ, de Paiva CS, Chauhan SK, et al. TFOS DEWS II pathophysiology report. Ocul Surf. 2017;15:438-510.
Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15:276-283.
Stapleton F, Alves M, Bunya VY, et al. TFOS DEWS II epidemiology report. Ocul Surf. 2017;15:334-365.
Wolffsohn JS, Arita R, Chalmers R, et al. TFOS DEWS II diagnostic methodology report. Ocul Surf. 2017;15:539-574.
The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop. Ocul Surf. 2007;5:75-92.
Methodologies to diagnose and monitor dry eye disease: report of the Diagnostic Methodology Subcommittee of the International Dry Eye WorkShop. Ocul Surf. 2007;5:108-152.
Research in dry eye: report of the Research Subcommittee of the International Dry Eye WorkShop. Ocul Surf. 2007;5:179-193.
Nelson JD, Craig JP, Akpek EK, et al. TFOS DEWS II introduction. Ocul Surf. 2017;15:269-275.
Jacobi C, Jacobi A, Kruse FE, Cursiefen C. Tear film osmolarity measurements in dry eye disease using electrical impedance technology. Cornea. 2011;30:1289-1292.
Messmer EM, Bulgen M, Kampik A. Hyperosmolarity of the tear film in dry eye syndrome. Dev Ophthalmol. 2010;45:129-138.
Tomlinson A, Khanal S, Ramaesh K, Diaper C, McFadyen A. Tear film osmolarity: determination of a referent for dry eye diagnosis. Invest Ophthalmol Vis Sci. 2006;47:4309-4315.
Muselier-Mathieu A, Bron AM, Mathieu B, et al. Ocular surface assessment in soft contact lens wearers; the contribution of tear osmolarity among other tests. Acta Ophthalmol. 2014;92:364-369.
Carney LG, Hill RM. Human tear pH. Diurnal variations. Arch Ophthalmol. 1976;94:821-824.
du Toit R, Vega JA, Fonn D, Simpson T. Diurnal variation of corneal sensitivity and thickness. Cornea. 2003;22:205-209.
Shen M, Wang J, Tao A, et al. Diurnal variation of upper and lower tear menisci. Am J Ophthalmol. 2008;145:801-806.
Lemp MA, Bron AJ, Baudouin C, et al. Tear osmolarity in the diagnosis and management of dry eye disease. Am J Ophthalmol. 2011;151:792-798 e791.
Urzua CA, Vasquez DH, Huidobro A, Hernandez H, Alfaro J. Randomized double-blind clinical trial of autologous serum versus artificial tears in dry eye syndrome. Curr Eye Res. 2012;37:684-688.
Gokhale M, Stahl U, Jalbert I. In situ osmometry: validation and effect of sample collection technique. Optom Vis Sci. 2013;90:359-365.
Keech A, Senchyna M, Jones L. Impact of time between collection and collection method on human tear fluid osmolarity. Curr Eye Res. 2013;38:428-436.
Nolfi J, Caffery B. Randomized comparison of in vivo performance of two point-of-care tear film osmometers. Clin Ophthalmol. 2017;11:945-950.
Sullivan B. Challenges in using signs and symptoms to evaluate new biomarkers of dry eye disease. Ocul Surf. 2014;12:2-9.
Sullivan BD, Whitmer D, Nichols KK, et al. An objective approach to dry eye disease severity. Invest Ophthalmol Vis Sci. 2010;51:6125-6130.
Pena-Verdeal H, Garcia-Resua C, Ramos L, Yebra-Pimentel E, Giraldez MJ. Diurnal variations in tear film break-up time determined in healthy subjects by software-assisted interpretation of tear film video recordings. Clin Exp Optom. 2016;99:142-148.
Miller KL, Walt JG, Mink DR, et al. Minimal clinically important difference for the ocular surface disease index. Arch Ophthalmol. 2010;128:94-101.
Glasson MJ, Stapleton F, Keay L, Sweeney D, Willcox MD. Differences in clinical parameters and tear film of tolerant and intolerant contact lens wearers. Invest Ophthalmol Vis Sci. 2003;44:5116-5124.
Nichols KK, Mitchell GL, Zadnik K. The repeatability of clinical measurements of dry eye. Cornea. 2004;23:272-285.
Nichols KK, Nichols JJ, Mitchell GL. The lack of association between signs and symptoms in patients with dry eye disease. Cornea. 2004;23:762-770.
Bron AJ, Evans VE, Smith JA. Grading of corneal and conjunctival staining in the context of other dry eye tests. Cornea. 2003;22:640-650.
Garcia-Resua C, Santodomingo-Rubido J, Lira M, Giraldez MJ, Vilar EY. Clinical assessment of the lower tear meniscus height. Ophthalmic Physiol Opt. 2009;29:487-496.
Johnson ME, Murphy PJ. The agreement and repeatability of tear meniscus height measurement methods. Optom Vis Sci. 2005;82:1030-1037.
Aslan Bayhan S, Bayhan HA, Muhafiz E, Bekdemir S, Gurdal C. Effects of osmoprotective eye drops on tear osmolarity in contact lens wearers. Can J Ophthalmol. 2015;50:283-289.
Dimit R, Miller W, Leach N, Bergmanson J. Comparison of morning and afternoon osmolarity in silicone hydrogel wearers and non-contact lens wearers. Invest Ophthalmol Vis Sci. 2011;52:6538.
Li M, Du C, Zhu D, Shen M, Cui L, Wang J. Daytime variations of tear osmolarity and tear meniscus volume. Eye Contact Lens. 2012;38:282-287.
Oncel BA, Pinarci E, Akova YA. Diurnal variation of the tear osmolarity in normal subjects measured by a new microchip system. Eur J Ophthalmol. 2012;22 Suppl 7:S1-S4.
Yiğit U, Evcimen Y, Kırık F, Ağaçhan A. Daytime variations of tear osmolarity measurement in dry eyes patients (article in turkish). Turk J Ophthalmol 2013;43:437-441.
Armstrong RA, Davies LN, Dunne MC, Gilmartin B. Statistical guidelines for clinical studies of human vision. Ophthalmic Physiol Opt. 2011;31:123-136.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307-310.
Farris RL, Stuchell RN, Mandel ID. Tear osmolarity variation in the dry eye. Trans Am Ophthalmol Soc. 1986;84:250-268.
Garcia N, Teson M, Enriquez-de-Salamanca A, et al. Basal values, intra-day and inter-day variations in tear film osmolarity and tear fluorescein clearance. Curr Eye Res. 2014;39:673-679.
Liu H, Begley C, Chen M, et al. A link between tear instability and hyperosmolarity in dry eye. Invest Ophthalmol Vis Sci. 2009;50:3671-3679.
Stahl U, Willcox M, Stapleton F. Osmolality and tear film dynamics. Clin Exp Optom. 2012;95:3-11.
Luo L, Li DQ, Pflugfelder SC. Hyperosmolarity-induced apoptosis in human corneal epithelial cells is mediated by cytochrome c and MAPK pathways. Cornea. 2007;26:452-460.
Sullivan BD, Crews LA, Messmer EM, et al. Correlations between commonly used objective signs and symptoms for the diagnosis of dry eye disease: clinical implications. Acta Ophthalmol. 2014;92:161-166.
Potvin R, Makari S, Rapuano CJ. Tear film osmolarity and dry eye disease: a review of the literature. Clin Ophthalmol. 2015;9:2039-2047.
Ray WA, O’Day DM. Statistical analysis of multi-eye data in ophthalmic research. Invest Ophthalmol Vis Sci. 1985;26:1186-1188.
Versura P, Profazio V, Campos EC. Performance of tear osmolarity compared to previous diagnostic tests for dry eye diseases. Curr Eye Res. 2010;35:553-564.
Benjamin WJ, Hill RM. Human tears: osmotic characteristics. Invest Ophthalmol Vis Sci. 1983;24:1624-1626.
Dalton K, Jones L. The performance of a novel nanolitre osmometer to investigate diurnal tear film osmolality. Optom Vis Sci 2005; 82. E-abstract 0557070.
Lee YB, Koh JW, Hyon JY, Wee WR, Kim JJ, Shin YJ. Sleep deprivation reduces tear secretion and impairs the tear film. Invest Ophthalmol Vis Sci. 2014;55:3525-3531.
Niimi J, Tan B, Chang J, et al. Diurnal pattern of tear osmolarity and its relationship to corneal thickness and deswelling. Cornea. 2013;32:1305-1310.
Himebaugh NL, Begley CG, Bradley A, Wilkinson JA. Blinking and tear break-up during four visual tasks. Optom Vis Sci. 2009;86: E106-E114.
Torricelli AA, Novaes P, Matsuda M, et al. Correlation between signs and symptoms of ocular surface dysfunction and tear osmolarity with ambient levels of air pollution in a large metropolitan area. Cornea. 2013;32:e11-e15.
Garcia N, Melvi G, Pinto-Fraga J, Calonge M, Maldonado MJ, Gonzalez-Garcia MJ. Lack of agreement among electrical impedance and freezing-point osmometers. Optom Vis Sci. 2016;93:482-487.
Pena-Verdeal H, Garcia-Resua C, Minones M, Giraldez MJ, Yebra-Pimentel E. Accuracy of a freezing point depression technique osmometer. Optom Vis Sci. 2015;92:e273-e283.
Benjamin WJ, Hill RM. Tear osmotic differences across the ocular surface. Graefes Arch Clin Exp Ophthalmol. 1986;224:583-586.
Copyright (c) 2020 Hugo Pena-Verdeal, Covadonga Vazquez-Sanchez, Jacobo Garcia-Queiruga, Carlos Garcia-Resua

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- Authors retain copyright and grant the journal right of first publication, with the work twelve (12) months after publication simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal.
- Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgement of its initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See The Effect of Open Access).