Contrast sensitivity before and after small incision lenticule extraction and femtosecond laser in situ keratomileusis
Abstract
Introduction: Contrast sensitivity function after laser ablation of the cornea in refractive surgery is an important tool for measuring quality of visual function. The effect of small incision lenticule extraction (SMILE) and femtosecond laser in situ keratomileusis (FS-LASIK) on visual function can be compared by measuring spatial contrast sensitivity.
Purpose: This study was to compare contrast sensitivity function in patients undergoing refractive surgery for myopia at Tilganga Institute of Ophthalmology.
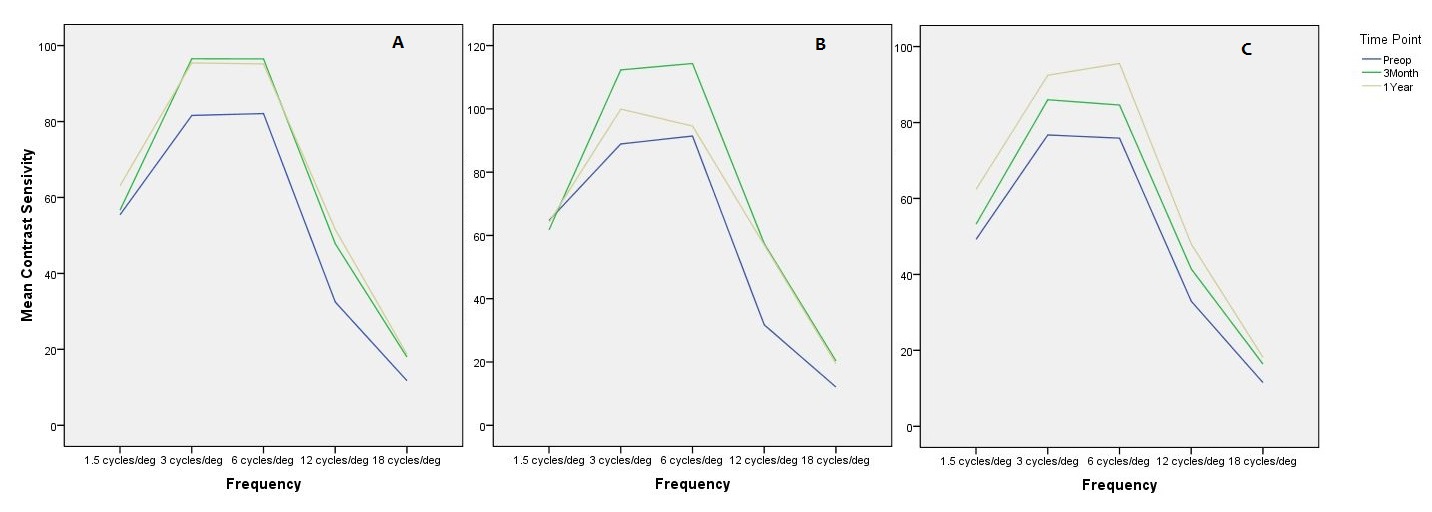
Methods: In a retrospective study, 15 subjects who underwent refractive surgeries comprising 9 cases of SMILE and 6 cases of FS-LASIK at Tilganga Eye Hospital were enrolled in the study. A major assessment included best corrected monocular contrast sensitivity with functional vision analyzer at spatial frequencies of 1.5, 3, 6, 12, and 18 cycles/deg in photopic condition (85 cd/m2) before, 3 months, and 1 year after the surgery. The average functional acuity contrast test scores for each spatial frequency were recorded. Differences between preoperative and postoperative contrast sensitivity at each spatial frequency were analyzed through parametric paired Student’s t-test.
Results: Contrast sensitivity of postoperative FS-LASIK and SMILE did not differ from preoperative values at a photopic level. However, at high spatial frequency (12 and 18 cycles/deg), contrast sensitivity function improved significantly (p < 0.05) in eyes after FS-LASIK. Eyes after SMILE surgery did not show any reduction in contrast sensitivity at all the spatial frequencies.
Conclusion: Under photopic conditions, the contrast sensitivity function is unaffected by SMILE or FS-LASIK.
References
Lohmann CP, Garty DS, Muir MK, Timberlake GT, Fitzke FW, Marshall J. Corneal haze after excimer laser refractive surgery: objective measurements and functional implications. Eur J Ophthalmol. 1991;1:173-180.
Ficker LA, Bates AK, Steele AD, et al. Excimer laser photorefractive keratectomy for myopia: 12 months follow-up. Eye. 1993;7:617-624.
Dutt S, Steinert RF, Raizman MB, Puliafito CA. One-year results of excimer laser photorefractive keratectomy for low to moderate myopia. Arch Ophthalmol. 1994;112:1427-1436.
Ambrosio G, Cennamo G, De Marco R, Loffredo L, Rosa N, Sebastiani A. Visual function before and after photorefractive keratectomy for myopia. Refract Corneal Surg. 1994;10:129-136.
Butuner Z, Elliott DB, Gimbel HV, Slimmon S. Visual function one year after excimer laser photorefractive keratectomy. Refract Corneal Surg. 1994;10:625-630.
Halliday BL. Refractive and visual results and patients satisfaction after excimer laser photorefractive keratectomy for myopia. Br J Ophthalmol. 1995;79:881-887.
Lafond G. Treatment of halos after photorefractive keratectomy. J Refract Surg. 1997;13:83-88.
Ghaith AA, Danile J, Stulting RD, Thompson KP, Lynn M. Contrast sensitivity and glare disability after radial keratotomy and photorefractive keratectomy. Arch Ophthalmol. 1998;116:12-18.
Holladay JT, Dudeja DR, Chang J. Functional vision and corneal changes after laser in situ keratomileusis determined by contrast sensitivity, glare testing, and corneal topography. J Cataract Refract Surg. 1999;25:663-669.
Nordan LT, Slade SG, Baker RN, Suarez C, Juhasz T, Kurtz R. Femtosecond laser flap creation for laser in situ keratomileusis: six-month follow-up of initial U.S. clinical series. J Refract Surg. 2003;19:8-14.
Kim JY, Kim MJ, Kim TI, Choi HJ, Pak JH, Tchah H. A femtosecond laser creates a stronger flap than a mechanical microkeratome. Invest Ophthalmol Vis Sci. 2006;47:599-604.
Binder PS. One thousand consecutive IntraLase laser in situ keratomileusis flaps. J Cataract Refract Surg. 2006;32:962-969.
Montes-Micó R, RodrÃguez-Galietero A, Ali ó JL. Femtosecond laser versus mechanical keratome LASIK for myopia. Ophthalmology. 2007;114:62-68.
Sugar A. Ultrafast (femtosecond) laser refractive surgery. Curr Opin Ophthalmol. 2002;13:246-249.
Krueger RR, Trokel SL, Schubert HD. Interaction of ultraviolet laser light with the cornea. Invest Ophthalmol Vis Sci. 1985;26:1455-1464.
Pellin MJ, Williams GA, Young CE, Gruen DM, Peters MA. Endoexcimer laser intraocular ablative photodecomposition. Am J Ophthalmol. 1985;99:483-484.
Marshall J, Sliney DH. Endoexcimer laser intraocular ablative photodecomposition. Am J Ophthalmol. 1986;101:130-131.
McDonald MB, Deiz MR, Frantz JM, et al. Photorefractive keratectomy for low-to-moderate myopia and astigmatism with a small-beam, tracker-directed excimer laser. Ophthalmology. 1999;106:1481-1488.
Shah R, Shah S. Effect of scanning patterns on the results of femtosecond laser lenticule extraction refractive surgery. J Cataract Refract Surg. 2011;37:1636-1647.
Reinstein DZ, Archer TJ, Gobbe M. Small incision lenticule extraction (SMILE) history, fundamentals of a new refractive surgery technique and clinical outcomes. Eye Vision. 2014;1:3.
Van den Berg TJ. Importance of pathological intraocular light scatter for visual disability. Doc Ophthalmol. 1986;61:327-333.
Wachler BS, Durrie DS, Assil KK, Krueger RR. Role of clearance and treatment zones in contrast sensitivity: significance in refractive surgery. J Cataract Refract Surg. 1999;25:16-23.
Montés-Micó R, Charman WN. Mesopic contrast sensitivity function after excimer laser photorefractive keratectomy. J Refract Surg. 2002;18:9-13.
Montés-Micó R, Charman WN. Choice of spatial frequency for contrast sensitivity evaluation after corneal refractive surgery. J Refract Surg. 2001;17:646-651.
Montés-Micó R, España E, Menezo JL. Mesopic contrast sensitivity function after laser in situ keratomileusis. J Refract Surg. 2003;19:353-356.
Pérez-Santonja JJ, Sakla HF, Alió JL. Contrast sensitivity after laser in situ keratomileusis. J Cataract Refract Surg. 1998;24:183-189.
Huang SCM, Chen HCJ. Overview of laser refractive surgery. Chang Gung Med J. 2008;31:237-252.
Tuan KM, Liang J. Improved contrast sensitivity and visual acuity after wavefront-guided laser in situ keratomileusis: in-depth statistical analysis. J Cataract Refract Surg. 2006;32(2):215-20.
Copyright (c) 2019 Asik Pradhan, Gauri Shankar Shrestha

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- Authors retain copyright and grant the journal right of first publication, with the work twelve (12) months after publication simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal.
- Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgement of its initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See The Effect of Open Access).